Digital Health to Support Family Planning Providers: Improving knowledge, capacity, and service quality
What is the program enhancement that can intensify the impact of High Impact Practices in Family Planning?
Use digital technologies to support service providers in delivering quality contraceptive services.

Nukua'lofa, Tonga Photo: Tom Perry / World Bank
Background
Used by appropriately trained health care providers and with supportive processes in place, devices such as mobile phones, tablets, and computers with various software applications are equipping countries to improve health care delivery, strengthen health systems, and support clients. With growing evidence that technologies can yield time and resource efficiencies and improve quality of care—resulting in better patient outcomes—in 2019 the World Health Organization (WHO) issued recommendations for digital interventions for health systems strengthening.1
This brief uses the WHO definition of digital health from the draft Global Strategy on Digital Health 2020-20242: “the field of knowledge and practice associated with the development and use of digital technologies to improve health.” Therefore, the recommendations here include interventions in mHealth (medical and public health practice supported by mobile devices) and eHealth (the use of information and communication technologies for health), with the most recent evidence largely focused on mHealth.
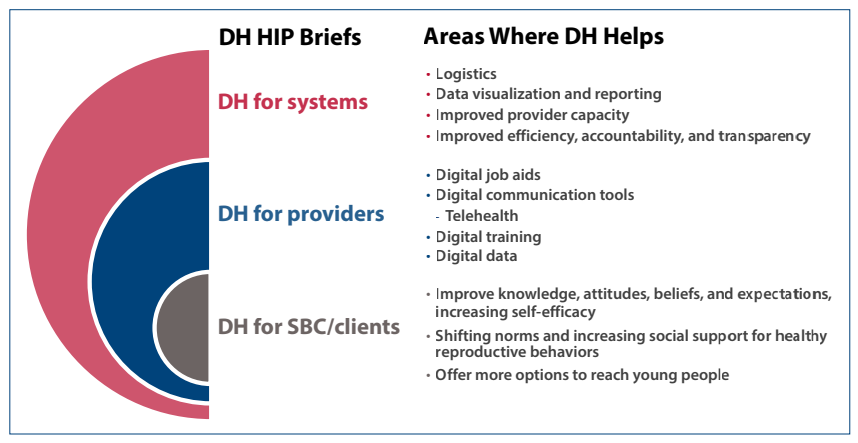
Of the six building blocks of health systems identified by the WHO,3 this brief focuses on the first: service delivery. More specifically the focus is on the ways digital health can support service providers to deliver quality contraceptive services. In context of the more recent high-quality health system framework, this brief focuses on two aspects of the framework: competent care and systems (process of care element) and workforce (foundations element).4 The focus of the brief is specifically on providers because other High Impact Practice (HIPs) briefs discuss digital health for social and behavior change and digital health for systems. Figure 1 summarizes content included in the three digital health HIPs briefs.
Digital Health (DH) HIPs Briefs
Frontline health workers in communities and primary care facilities play a vital role in the provision of family planning (FP), as they are uniquely poised to shape health outcomes.5 A growing body of evidence indicates the use of digital tools by providers supports a range of functions, including registration, health data collection and reporting to improve continuity of care, and improved adherence to treatment approaches. Indeed, use of digital tools by providers promotes consistent and successful adherence to evidence-based service delivery protocols.6 While evidence specific to digital tools’ impact on FP outcomes is limited, results from other health areas are likely generalizable to FP programming.1
Digital health tools can help FP providers deliver a higher quality of care through job aids, communication tools, training, and data. The Theory of Change (Figure 2) shows systems-level outcomes and client-level impacts when providers use digital health tools to address barriers to quality of service.
Theory of Change

Digital Health to Support Family Planning Providers has been identified as an enhancement to High Impact Practices in Family Planning (HIPs) by the HIPs technical advisory group. An “enhancement” is a practice that can be implemented in conjunction with HIPs to further intensify the impact of the HIPs. For more information about HIPs, see https://fphighimpactpractices.org/overview.
How can digital technologies enhance HIPs?
A review of the literature shows that four digital health enhancements for providers in particular may increase the quality of FP services: 1) digital job aids, 2) digital communication tools, 3) digital training, and 4) digital data. Details on how these digital tools can help FP providers appear below, with examples of each tool provided in Table 1. Note that while some evidence suggests the impact of digital health interventions on FP services, limited research exists on the cost-effectiveness of these approaches. Thus, information on cost-effectiveness is not included in this section and a question on cost-effectiveness is included in the “priority research questions” section of this brief.
Digital job aids: Also called digital clinical decision support systems (CDSS), these can be accessed via mobile phones or tablets. Digital job aids can enhance the quality of FP programs by helping to improve service providers’ adherence to clinical protocols through use of digital checklists, counseling and treatment algorithms, and appropriate patient-specific clinical recommendations. Mobile phones, for example, can serve as a digital job aid to support providers’ interactions with FP clients. They can also be used to refer FP clients to specific clinical services for provision of contraceptive methods not offered by those providers. Not only does this facilitate efficient linkage to family planning services, but it can also support longitudinally tracking clients’ completion of referrals and method use.7 This can allow providers to better support client follow-up.
Digital communication tools: Digital communication tools facilitate communication between providers and supervisors or providers and clients by using functions such as SMS and interactive voice response (IVR), as well as online communication platforms such as Zoom. Digital applications may enhance FP programs by offering an efficient means to provide supportive supervision remotely and to solicit honest feedback from clients. Use of remote communication via SMS and mobile-based modules can promote more frequent and less labor-intensive supervision than in-person consultation. For client feedback on service quality that can be readily used by FP service providers to enhance service quality, digital tools such as SMS and IVR surveys can be effective approaches for follow-up, but careful assessment of client phone ownership trends and usage patterns is recommended. Women, in particular, are more likely to have access to a shared phone than to own a personal device, which may compromise their privacy when responding to a survey on FP service quality. Installing tablets in clinic waiting rooms, rather than using paper-based surveys and client exit interviews, is another digital approach which may offer efficiencies on the collection of data on the quality of FP services. This technology allows for data review in real-time and faster correction of errors, as well as for rapid feedback cycles without the burden of manual data entry. As the information is entered by the clients, software can facilitate transformation of the data into a usable electronic data format. Furthermore, data interfaces can generate dashboards that give health providers access to easily digestible information rather than raw data. Data collection via tablets can also offer more privacy than a human-administered exit interview.
Telehealth, which entails providing health care remotely through various communication tools,8,9 is another important digital communication tool emerging within FP programs, particularly in light of the 2020 COVID-19 pandemic. While telehealth is primarily understood as benefiting clients by helping them to overcome barriers to accessing health care,8,10 client-to-provider telehealth can also benefit providers by allowing providers the flexibility to reach clients separated by distance,1 including in their own homes. Provider-to-provider telehealth can facilitate communication between providers for consultations on case management, requesting second opinions, or coordinating care.1 While there is limited evidence on the use of telemedicine to support FP counseling and service provision in low- and middle-income countries, an analysis of access to contraceptives through a telehealth platform in the United States revealed that while it can increase contraceptive access for women in rural areas,10 its overall use was not common.11 Another analysis by the Kaiser Family Foundation found that only 0.02% of all reproductive health claims in the 2017 IBM Health Analytics MarketScan Commercial Claims and Encounters Database from the USA were related to telemedicine.12 These studies suggest that telemedicine holds promise, but that even in developed contexts it is an underutilized tool for the provision of reproductive health. Indeed, it requires careful planning, including training and accrediting health providers,13 and demand creation.
Digital training: Appropriate service provider trainings are one of the cornerstones of a high-quality FP program. As a complement to in-person trainings, digital applications can improve clinical and non-clinical knowledge through refresher trainings and continuous learning opportunities for various cadres of service providers.14 Multimedia eLearning courses and IVR facilitate “on demand” training and access to content and technical resources while not requiring providers to leave facilities. Programmatic experience indicates that a tablet-based system utilized by social franchise networks—including pharmacies and drug shops—can provide performance feedback and coaching information to FP service providers while also monitoring performance over time, thus enhancing service quality.15
Digital data: Real-time collection of client data and appropriate access to client data can aid in continuity of care at the individual level and efficient resource planning at the population level. Digital data may also provide more granular and higher-quality data when compared with analog data, and digital tools can expedite the aggregation of data to “near-instantaneous reporting.”16 This can provide FP providers with faster access to data to enhance service quality. The benefits for service providers include real-time visibility into patient information, including historic and current health data accessible via a dashboard, enabling new insights as well as prompts and reminders for providers.14,16 Finally, timely data about contraceptive supplies can help manage logistics and therefore reduce stockouts. Further information on the use of digital data to prevent stockouts and enhance supply chain functions can be found in the Digital Health for Systems HIPs brief.
Examples of digital tools for providers
| Digital Tools | Examples from low- and middle-income countries |
|---|---|
| Job aids |
|
| Communication tools |
|
| Training |
|
| Data |
|
How to do it: Tips from implementation experience
As outlined in the WHO guideline Recommendations on Digital Interventions for Health Systems Strengthening,1 “implementations need to be made appropriate to the local needs, intended users, and overall ecosystem comprised of the information and communications technology (ICT) and enabling environment.” While the percent of internet users around the world has been rapidly increasing in the past 14 years from 16.8% in 2005 to 53.6% in 2019,27 the increase has not occurred at the same pace in all countries nor in all regions within countries. Typically, well-resourced urban areas are the first to receive faster, next-generation cellular networks, whereas poorer, rural areas lag behind. This situation can exacerbate inequities because more data will be collected in advantaged areas compared to disadvantaged areas, thereby placing more emphasis on problems in advantaged areas. Likewise, those communities with better infrastructure will reap the benefits of earlier access to new findings and new treatments. Governments, donors, and program managers should seek to address these issues with upfront investments to support expanded network coverage and other infrastructure, as well as flexible implementation periods needed to support health facilities’ transitions between analog and new digital systems.
Several resources exist for countries seeking to implement digital health interventions, including the National eHealth Strategy Toolkit by WHO and the International Telecommunication Union to help countries determine their readiness to adopt digital health interventions ,28 USAID’s guidance in Accelerating the Journey to Self-Reliance Through Strategic Investments in Digital Technologies,29 and the MEASURE Evaluation tool to guide decisions on security, privacy, and confidentiality of personal health information collected and managed using mobile devices.30 Any initiatives to pursue digital product development should begin by reviewing the “Principles for Digital Development,”31 the aforementioned MEASURE Evaluation tool, and other general digital development resources. This will help to ensure that digital products are designed with the intended user in mind, built for sustainability and scale, and when possible, constructed using existing platforms and products. Digital health solutions for providers may require upfront investments on the hardware (e.g., phones, tablets, servers) and software (e.g., trainings, dashboards), as well as ongoing maintenance. Successful implementation of digital health solutions will depend upon careful planning for these initial costs. Table 2 offers tips specific to the four digital health applications discussed earlier.
Tips for digital health enhancements for family planning service providers.
| Digital health enhancement | Tips when designing and implementing |
|---|---|
| Digital job aids | Design:
Quality Assurance:
Training:
|
| Digital communication tools | Design:
Quality Assurance:
|
| Digital training | Design:
Quality Assurance:
|
| Digital data | Quality Assurance:
Training:
|
* Back-end data is the data that users of an application don't see in their day-to-day interaction with the application. Back-end data includes pieces of information like what time of day an application was used, how long the user engaged with the application, which features of an application a user selects, etc. This information is usually captured by the application itself and accessed by an administrator.
Indicators
Outcome-focused indicators by type of tool:
- Decision-support tools and digital provider communication and performance feedback: % of providers with improved adherence to service delivery protocols
- Digital/remote training: % of providers with improved knowledge and/or competence
Priority research questions
- Do digital applications that support family planning providers contribute to client-level outcomes such as increase in modern contraceptive prevalence rate?
- Which digital health interventions for family planning providers are most cost-effective?
- How can governments invest in digital health technology to support health providers’ work in a way that doesn’t exacerbate inequity, with rural communities being denied the full benefits of digital health interventions due to inconsistent coverage and access?
Tools and resources
- Digital Health Atlas, search for “family planning” or country of interest33: Provides a map summarizing digital health interventions in various countries, facilitating planning, coordination, and use of digital health information systems.
- CHW Maturity Model and Toolkit34: Allows programs to design a pathway to implement scalable digital health programs to advance community health.
- WHO Digital Accelerator Kits (Family Planning): They distill WHO guidelines in a digital format to assist providers so that they can more readily use them.
Search Strategy
To compile the list of documents meeting inclusion criteria, a literature search was conducted using bibliographic databases and hand searching of online websites for peer-reviewed and grey literature. Evidence relevant to how digital technologies can support service providers to enhance High Impact Practices in Family Planning (HIPs) was systematically analyzed. The period of review focused on documents published between 2016 and 2019, i.e., following development of the previous HIPs brief on digital health.
For more information, download the “Methods for Literature Search, Information Sources, Abstraction, and Synthesis” document.
References
- World Health Organization (WHO). Recommendations on Digital Interventions for Health System Strengthening. WHO; 2019. Accessed November 24, 2020. https://www.who.int/reproductivehealth/publications/digital-interventions-health-system-strengthening/en/
- World Health Organization (WHO). Draft Global Strategy on Digital Health 2020-2024. WHO; 2020. Accessed November 24, 2020. https://www.who.int/docs/default-source/documents/gs4dh.pdf?sfvrsn=cd577e23_2
- World Health Organization (WHO). Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement Strategies. WHO; 2010. Accessed November 18, 2020. https://www.who.int/healthinfo/systems/WHO_MBHSS_2010_full_web.pdf
- Kruk ME, Gage AD, Arsenault C, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution [published correction appears in Lancet Glob Health. 2018 Sep 18;:] [published correction appears in Lancet Glob Health. 2018 Nov;6(11):e1162]. Lancet Glob Health. 2018;6(11):e1196-e1252. http://doi.org/10.1016/S2214-109X(18)30386-3.
- Agarwal S, Perry HB, Long LA, Labrique AB. Evidence on feasibility and effective use of mHealth strategies by frontline health workers in developing countries: systematic review. Trop Med Int Health. 2015;20(8):1003-1014. https://doi.org/10.1111/tmi.12525
- Celi LAG, Fraser HS, Osorio JS, Paik K, Nikore V. Global Health Informatics: Principles of eHealth and mHealth to Improve Quality of Care. MIT Press; 2017.
- Advancing Partners and Communities. Situation Analysis of Community-Based Referrals for Family Planning. JSI Research & Training Institute, Inc., Advancing Partners and Communities; 2016. Accessed November 19, 2020. https://www.advancingpartners.org/sites/default/files/technical-briefs/apc_situation_analysis_cbfp_brief.pdf
- Dorsey ER, Topol EJ. State of telehealth. N Engl J Med. 2016;375(2):154-161. https://doi.org/10.1056/NEJMra1601705
- Tuckson RV, Edmunds M, Hodgkins ML. Telehealth. N Engl J Med. 2017;377(16):1585-1592. https://doi.org/10.1056/NEJMsr1503323
- Sundstrom B, DeMaria AL, Ferrara M, Meier S, Billings D. “The Closer, the Better:” The Role of Telehealth in Increasing Contraceptive Access Among Women in Rural South Carolina. Matern Child Health J. 2019;23(9):1196-1205. https://doi.org/10.1007/s10995-019-02750-3
- Martinez KA, Rastogi R, Lipold L, Rothberg MB. Response to requests for contraception in one direct-to-consumer telemedicine service. Contraception. 2020;101(5):350-352. https://doi.org/10.1016/j.contraception.2020.01.017
- Weigel G, Frederiksen B, Ranji U, Salganicoff A. Telemedicine in Sexual and Reproductive Health. Kaiser Family Foundation; 2019. Accessed November 19, 2020. https://www.kff.org/womens-health-policy/issue-brief/telemedicine-in-sexual-and-reproductive-health/
- Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020;26(5):309-313. https://doi.org/10.1177/1357633X20916567
- Mitchell M, Kan L. Digital technology and the future of health systems. Health Syst Reform. 2019;5(2):113-120. https://doi.org/10.1080/23288604.2019.1583040
- Quality Improvement Within Social Franchise Networks. Accessed November 19, 2020. https://mis.psi.org/where-is-hnqis/?lang=en
- Labrique AB, Vasudevan L, Kochi E, Fabricant R, Mehl G. mHealth innovations as health system strengthening tools: 12 common applications and a visual framework. Glob Health Sci Pract. 2013;1(2):160-171. https://doi.org/10.9745/GHSP-D-13-00031
- Center for Human Services. Texting for Maternal Wellbeing: Use of Mobile Phones by CHWs to Offer Family Planning Services. Center for Human Resources; 2014. Accessed November 19, 2020. http://chwcentral.org/texting-maternal-wellbeing-use-mobile-phones-chws-offer-family-planning-services
- Borkum E, Sivasankaran A, Sridharan S, et al. (2015). Evaluation of the Information and Communication Technology (ICT) Continuum of Care Services (CCS) Intervention in Bihar. Mathemetica Policy Research; 2015. Accessed November 24, 2020. https://www.mathematica.org/our-publications-and-findings/publications/evaluation-of-the-information-and-communication-technology-ict-continuum-of-care-services-ccs
- Braun R, Lasway C, Agarwal S, et al. An evaluation of a family planning mobile job aid for community health workers in Tanzania. Contraception. 2016;94(1):27-33. https://doi.org/10.1016/j.contraception.2016.03.016
- Agarwal S, Lasway C, L’Engle K, et al. Family planning counseling in your pocket: a mobile job aid for community health workers in Tanzania. Glob Health Sci Pract. 2016;4(2):300-310. Published 2016 Jun 27. https://doi.org/10.9745/GHSP-D-15-00393
- Lemay NV, Sullivan T, Jumbe B, Perry CP. Reaching remote health workers in Malawi: baseline assessment of a pilot mHealth intervention. J Health Commun. 2012;17 Suppl 1:105-117. https://doi.org/10.1080/10810730.2011.649106
- Limaye RJ, Ballard Sara A, Ahmed N, et al. Enhancing the knowledge and behaviors of fieldworkers to promote family planning and maternal, newborn, and child health in Bangladesh through a digital health training package: results from a pilot study. Int Q Community Health Educ. 2020;40(2):143-149. https://doi.org/10.1177/0272684X19861866
- Limaye RJ, Kapadia-Kundu N, Arnold R, Gergen J, Sullivan TM. Utilizing digital health applications as a means to diffuse knowledge to improve family planning outcomes in Bangladesh. Clin Obstet Gynecol Reprod Med. 2017;3(2):1-7. https://doi.org/10.15761/COGRM.1000176
- Diedhiou A, Gilroy KE, Cox CM, et al. Successful mLearning pilot in Senegal: delivering family planning refresher training using interactive voice response and SMS. Glob Health Sci Pract. 2015;3(2):305-321. https://doi.org/10.9745/GHSP-D-14-00220
- Mohan D, Bashingwa JJH, Dane P, Chamberlain S, Tiffin N, Lefevre A. Use of big data and machine learning methods in the monitoring and evaluation of digital health programs in India: an exploratory protocol. JMIR Res Protoc. 2019;8(5):e11456. Published 2019 May 24. doi:10.2196/11456
- Tweya H, Feldacker C, Haddad LB, et al. Integrating family planning services into HIV care: use of a point-of-care electronic medical record system in Lilongwe, Malawi. Glob Health Action. 2017;10(1):1383724. https://doi.org/10.1080/16549716.2017.1383724
- United Nations, Telecommunication Development Sector (ITU-D). ITU Statistics. Accessed November 19, 2020. https://www.itu.int/en/ITU-D/Statistics/Pages/stat/default.aspx
- World Health Organization (WHO); International Telecommunication Union (ITU). National eHealth Strategy Toolkit. WHO and ITU; 2012. Accessed November 19, 2020. https://www.itu.int/dms_pub/itu-d/opb/str/D-STR-E_HEALTH.05-2012-PDF-E.pdf
- United States Agency for International Development (USAID). Accelerating the Journey to Self-Reliance Through Strategic Investments in Digital Technologies: A Digital-Health Vision for Action from the U.S. Agency for International Development. USAID; 2020. Accessed November 19, 2020. https://www.usaid.gov/global-health/health-systems-innovation/data/digital-health-vision
- Spigel L, Wambugu S, Villella C. mHealth Data Security, Privacy, and Confidentiality: Guidelines for Program Implementers and Policymakers. University of North Carolina at Chapel Hill, Carolina Population Center, MEASURE Evaluation; 2018. Accessed November 19, 2020. https://www.measureevaluation.org/resources/publications/ms-17-125a
- Principles for Digital Development. Accessed November 19, 2020. https://digitalprinciples.org/
- Measure Evaluation. Data Demand and Use. Accessed November 19, 2020. https://www.measureevaluation.org/our-work/data-demand-and-use
- World Health Organization. Digital Health Atlas. Accessed November 19, 2020. https://digitalhealthatlas.org/en/-/
- New Digital Health Tool Supports CHW Programs: Maturity Model and Toolkit. Accessed November 19, 2020. https://livinggoods.org/maturity-model/
Suggested citation
High Impact Practices in Family Planning (HIPs). Digital Health to Support Family Planning Providers: Improving knowledge, capacity, and service quality. Washington, DC: HIPs Partnership; 2020 Dec. Available from: https://fphighimpactpractices.org/briefs/digital-health-to-support-family-planning-providers/
Acknowledgements
This HIP enhancement was authored by Smisha Agarwal (JHSPH), Maria Carrasco (USAID), Lynn Heinisch (Independent Consultant), Nicole Ippoliti (YLabs), Manish Kumar (UNC-CH), Sam Wambugu (ICF), and Trinity Zan (FHI 360).
Critical review and helpful comments were provided by Kristina Celentano, Ramatu Daroda, Amy Finnegan, Ishrat Husain, Felicia Jones, Toshiko Kaneda, Joan Kraft, Shawn Malarcher, Leah McManus, Katie Meyer, Alex Mickler, Isaiah Ndong, Joseph Obure, Kaitlyn Patierno, Laura Raney, Vinit Sharma, Sara Stratton, Renata Tallarico, and Caitlin Thistle.
The World Health Organization/Department of Sexual and Reproductive Health and Research has contributed to the development of the technical content of HIPs briefs, which are viewed as summaries of evidence and field experience. It is intended that these briefs be used in conjunction with WHO Family Planning Tools and Guidelines: http://www.who.int/topics/family_planning/en/.
For more information about HIPs, please contact the HIPs team.
The HIPs represent a diverse and results-oriented partnership encompassing a wide range of stakeholders and experts. As such, the information in HIPs materials does not necessarily reflect the views of each co-sponsor or partner organization.