Supply Chain Management: Investing in the supply chain is critical to achieving family planning goals
High Impact Practice:
Invest in supply chain management by increasing data visibility and use, accelerating product flow, professionalizing the supply chain workforce, and capitalizing on private sector capacity.

In Nairobi, Kenya, a facility in-charge uses her phone and a system job aid to submit a monthly CDRR (consumption data report and request form) to the Tupange SMS commodity tracking system (TSCTS). © 2014 John Kihoro/Tupange(Jhpiego Kenya), Courtesy of Photoshare
Background
Stockouts of popular contraceptive products are common and persistent across many countries (Figure 1). A review of supply chain challenges in low- and middle-income countries (LMICs) concluded that various inefficiencies and bottlenecks across the supply chain contribute significantly to high stockout rates for modern contraceptives.1 Establishing and maintaining effective supply chain management is essential to making modern contraceptives available and thus helping individuals achieve their reproductive goals.2
Supply chain management organizes the vast network of supply chain players—procurers, manufacturers, shippers, distributors, warehouse agents, facility managers, and service providers—in a system to ensure timely delivery of products from the port, to central and sub-national warehouses, and ultimately to service delivery points and communities. An effective supply chain works when these players collaborate to make decisions on moving products, including how much to move, when, and how. To improve supply chain performance and increase product access, they need data visibility—information allowing them to jointly understand where products are in the system and which processes are blocking their movement. Figure 2 illustrates the interconnectedness between supply chain processes (i.e., forecasting and quantification, procurement, production, transportation, delivery) in the “end to end” supply chain, where a disruption at any point in the supply chain can result in lack of availability to the individual users at the service delivery point.
This brief focuses on key practices to strengthen the management of each step of the supply chain from the manufacturer to the service delivery point. Strengthening supply chains to meet the growing demand for family planning will require better data insight into product movement, strategic decisions to speed up product flows, adequate staffing and training, and consideration of how and when to leverage private sector supply chain expertise. As such, global health supply chain experts agree that the following four intervention areas will be key components to strengthening supply chain performance and meeting the product needs for family planning and other health programs:
- Increase data visibility and use for continuous improvement
- Speed up product flow through the supply chain
- Build and support a competent, professional supply chain workforce
- Capitalize on private sector supply chain capacity, where appropriate
Establishing and maintaining effective supply chain management, within the overall health system, is one of several “high-impact practices in family planning” (HIPs) identified by a technical advisory group of international experts.5 While sufficient financing and effective tendering procurement practices also play a significant role in family planning supply chains, these issues are addressed in the financing, commitment, and policy HIPs. For more information about other HIPs, see http://fphighimpactpractices.org/overview.
Percentage of facilities stocked out, by method offered, on the day of assessment

Source: FP2020 Core Indicator 10. 3
What challenges can a well-functioning supply chain help countries address?
Continuous availability of a wide range of contraceptive methods is a key factor in supporting an individual’s ability to plan and space pregnancies. Inadequate supplies of family planning commodities are estimated to account for up to one-third of the unmet need for family planning in LMICs.6 Lack of access and supply failures are among the most cited reasons in LMICs for unmet demand, non-use, and discontinuing contraception.7
A reliable stock of contraceptives supports voluntary choice—an important element in user satisfaction and method continuation. Contraceptive use is higher in contexts with a consistent supply of contraceptive method options. Data from East Africa indicate that a woman living in a region with one additional contraceptive method available in her region was 50% more likely to report using contraception than a woman living in a region with less choice.8 Similar findings have been documented in Haiti,9 Malawi,10 and Ethiopia.11
Effective supply chains support women’s choice of modern contraception and have the potential to meet latent demand for previously unavailable methods. This effect stems, in part, from improving quality of care and by reducing stockouts of needed contraceptive methods, as well as the ancillary supplies and equipment required for some clinical methods.7 It was exemplified by Senegal’s use of the informed push model (IPM), where nationwide consumption of modern contraception rose in one year by 48% due to the reliable availability of commodities.12
The various processes in the supply chain, from the service delivery point to warehouses to manufacturers, are linked in the “end to end” supply chain.
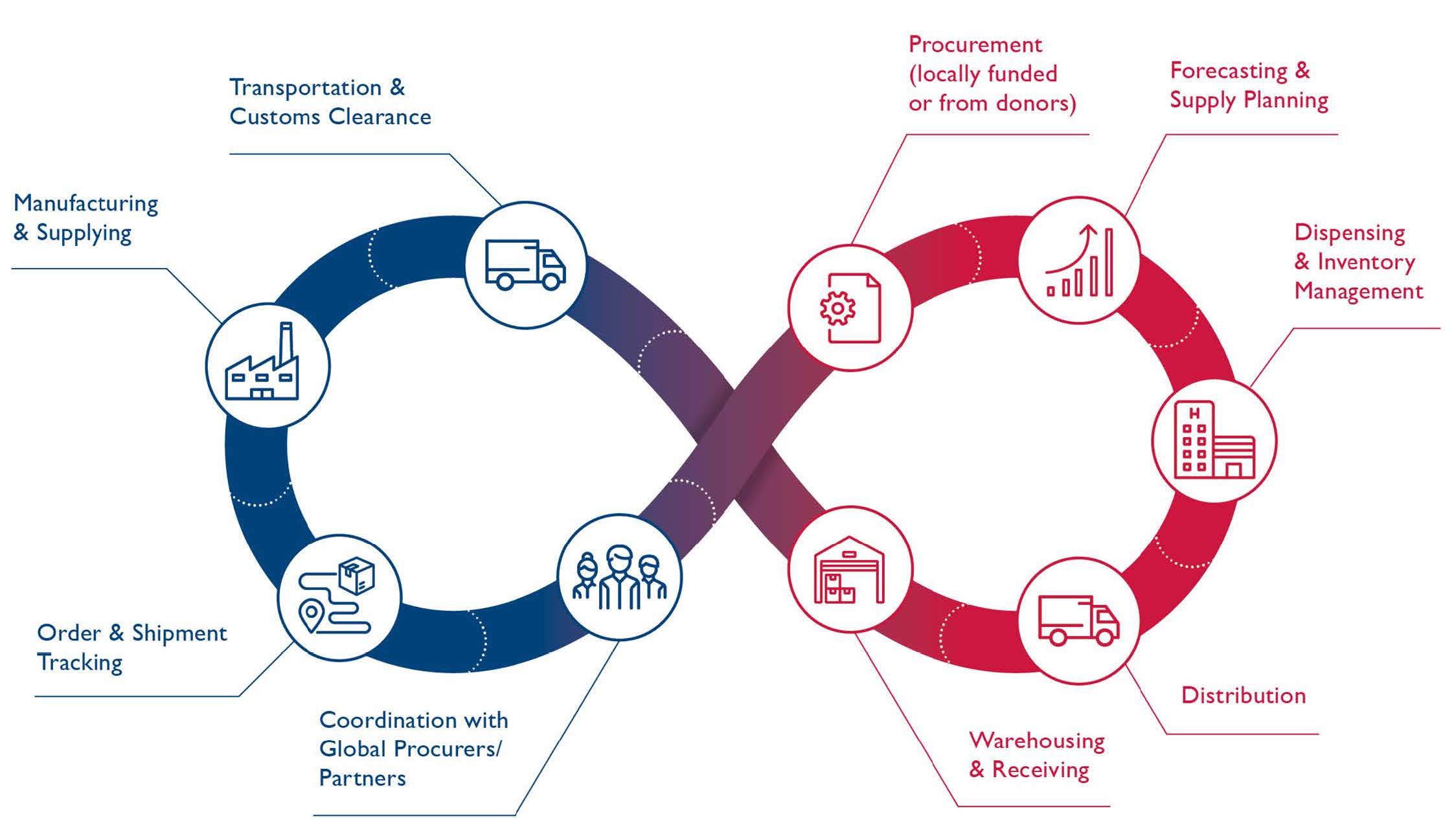
Source: Reproductive Health Supplies Coalition4
What is the evidence that a strong supply chain contributes to high impact family planning programs?
Increase data visibility and use for continuous improvement
How quickly and effectively family planning products move through the supply chain depends on a complex series of processes managed by different supply chain players across the globe, including forecasting, manufacturing, procurement, transportation, inventory management, and delivery. Collecting and analyzing the right data can offer the needed visibility to help governments, country partners, manufacturers, and global procurers make effective decisions related to estimating supply needs, procuring and distributing product, and advocating for adequate funding.13 In situations where global supply is scarce, systematic collection and sharing of supply chain data becomes even more critical to balance stock and coordinate shipments within and among countries. Supply chain data is also essential to continuous process and performance improvement, which are core aspects of supply chain strengthening programs.
Conducting routine supply chain assessments offers insights to identify and respond to process bottlenecks and is one of the fastest, most effective paths to improved supply chain performance.14,15 In Kaduna State, Nigeria, supply chain assessments in 2016 identified a “fragmented logistics data collection systems, duplication of efforts, wastages and significant losses in value for money.”16 Given the assessment findings, the State Government designed and launched the Kaduna State Public Health Supply Chain Transformation Project in 2017, based on the premise of systematically collecting and analyzing data to identify and resolve continued supply chain constraints. In 2017, the pilot reduced stockouts from 30% to 24%16.
Routine data collection from service delivery point stock and consumption is also important in order to help managers understand how much product is sitting in inventory versus being regularly consumed. Collecting and using such data in near real time has been proven to improve supply chain performance in private industry.17 In Kaduna State, in 2012, the United Nations Population Fund (UNFPA) supported bimonthly resupply meetings led by midwives that included the systematic review of data regarding each service delivery point’s stock levels, requisitions, and quantity distributed. A review found the approach reduced rates of stock unavailability and contributed to an approximate 50% increase in contraceptive consumption.18 In Tanzania, investments in a national logistics management unit and an electronic logistics management information system in 2014 increased use of service delivery point data and the accuracy of family planning forecasts, ultimately reducing the frequency and length of stockouts, and the proportion of product wasted due to expiration.19
Speed up product flow through the supply chain
The public health supply chains in many countries have three to four “tiers” (e.g., central, provincial, district, service, and delivery levels), with warehouses and storage at each level. The higher the number of tiers, the more inventory holding is required, which means the inventory spends more time “stopped” in warehouses. This increases supply chain costs, while leading to increased probability of damage, theft, expiries, and stockouts. Commercial distribution systems have streamlined their supply chains and increased the pace of distribution runs, significantly reducing stockouts at the point of consumption.20
Modeling studies have shown supply chains with fewer levels between the central agency and the service delivery points improve availability and in many cases also reduce costs.21,22 Streamlined supply chains lead to better information sharing between the levels in the distribution system, and improve accountability compared to supply chains with too many layers.23,24 Governments can improve supply chain efficiency and effectiveness through policy change to reduce the number of tiers, ideally using a network optimization process. Network optimization uses mathematical modeling to identify the best performing and most efficient number, size, and placement of warehouses for a supply chain. A network optimization exercise conducted in Mozambique indicated that consolidating two layers of the distribution system (with over 160 warehouses and storerooms) into a single intermediate level with 30 warehouses would save $6.7 million per year. The plans were formally approved in 2015 and the first intermediate warehouse was inaugurated in 2019.25 The continued implementation is expected to result in increased service levels and product availability, as well as reduced costs.
Mozambique and Zambia both revised and streamlined their reporting systems to allow demand and order data to flow directly from health facilities to the central distribution centers (as opposed to through districts and other layers in the system). Reducing the number of tiers involved in the information flow improves the speed at which information moves and establishes clearer responsibilities for reporting and action. In Mozambique, these improvements led to considerably higher product availability.26 In Zambia, direct flow of information from facilities to the central level, coupled with the central level preparing shipments for each facility, improved availability of various essential medicines, including contraceptives.23
Build and support a competent, professional supply chain workforce
For contraceptive and health product supply chains to succeed in fulfilling their mission, they must be managed and operated by a competent supply chain workforce that has the resources and support required to fulfill their responsibilities. Many government organizations find it difficult to recruit and retain qualified supply chain staff, and ministries of health often have insufficient human resources dedicated to the medicine supply chain. In Ghana, for example, lack of trained health workers greatly impeded distribution of modern contraceptives.27 The global health community recommends supply chain workers be recognized and included within existing human resources systems, including appropriate recruitment, support, motivation, and professional development and retention plans.28 Public sector organizations are encouraged to leverage the private sector to improve performance and reduce costs, rather than building all supply chain capabilities in-house (see next section).
While evidence on the impact in this area remains nascent and primarily from the private sector,29 the logical framework is strong and new research is being conducted in the global health area.28 Initial evidence from Nepal indicates that supply chain improvement efforts, including strategic outsourcing and institutionalized development of staff capacity, led to a reduction in contraceptive stockouts from 8% to less than 2%.30 Namibia and Ethiopia have also reported benefits to the overall health product supply chain as a result of systematic investment in designing supply chain workforce plans.31,32
A critical workforce factor for strong supply chain management is health sector leadership that recognizes and internalizes the importance of the supply chain to achieve health system goals, and the value of a capable and professional supply chain workforce. Supply chain leaders within the health system need to be elevated to strategic roles, and empowered within those roles to successfully advocate for supply chain needs and proactively address supply chain challenges. A strong leadership environment within the supply chain will promote excellence and attract talent, helping to address other workforce challenges.33,34

Photo credit: Reproductive Health Supplies Coalition
Capitalize on private sector supply chain capacity, where appropriate
The commercial sector brings unique supply chain capabilities and can play an important role in strengthening supply chains for health products. While the exact role varies depending on a country’s specific supply chain,35 contracting transport and distribution to private companies has yielded benefits in many countries (e.g., South Africa36; Senegal12,37). A notable example is a distribution outsourcing arrangement in Senegal, which reduced the proportion of health facilities experiencing stockouts from over 80% to less than 2%, while reducing annual distribution costs by 36%.12,37
Success of private sector engagement and contracting models has depended on a clear policy framework; strong government understanding and commitment, including contract management capacity in government; and a competitive local market for high-quality private supply chain service providers. Even in instances where the private sector cannot be leveraged for transportation, distribution, or other supply chain services, it can act as a source of technical best practices in designing and operating supply chains and their corresponding performance management systems.35
In many upper- and middle-income countries, retail pharmacies serve as health product access points even for public sector services, leveraging strong private sector pharmaceutical networks. In low income countries, family planning programs have a long history of providing contraceptives to individuals through private sector pharmacies and drug shops, which typically purchase contraceptives directly from private sector wholesalers or distributors. Opportunities may exist for expanding use of private sector pharmacies and drug shops as an integral part of the public sector family planning services to expand access in both rural and urban areas, possibly leveraging vouchers or subsidies.38,39
How to do it: Tips from implementation experience
Increase data visibility and use for continuous improvement
- Conduct regular and systematic assessments to identify supply chain bottlenecks and solutions. There are a number of tools available that can work separately or in conjunction. These tools can identify short-term “quick win” improvements, medium-term strategic level resource planning, and long-term comprehensive supply chain changes. The Technical Review of Public Health Supply Chain Assessment Tools can be used in selecting the most relevant assessment approaches.40 Regardless of the tools chosen for assessment, ultimately, the government and other key stakeholders should lead a process to distill the findings into one agreed vision for supply chain strengthening.
- Strengthen existing data collection while working toward electronic systems. It is not necessary to wait for the perfect electronic data system to benefit from data visibility. Existing data, such as service delivery point stock, months of stock, and average monthly consumption, can and should be analyzed to inform decision-making. Review of existing data collection tools and processes should be part of the supply chain assessments outlined above to identify opportunities to improve data quality and use. Once existing data collection processes are proven, and as the supply chain matures, data collection and use should evolve to automated, more advanced electronic processes that allow faster analysis.
- Adopt an electronic logistics management information system to work toward visibility across the whole supply chain, from manufacturers to service delivery points. Electronic data collection and systems allow frequent sharing of updates related to purchase orders, stock inventory, product consumption, and shipment and delivery statuses across a complex network of supply chain players. In situations where global supply is scarce, electronic systems make it easier to balance stock and coordinate shipments. Governments that put in place national electronic logistics management information systems, like the Tanzania example described above, can connect to electronic networks (e.g., the Global FP Visibility and Analytics Network)41 linking them to their global manufacturers and shippers. Countries can look to early adopters like Nigeria and Malawi for advice on connecting to global visibility networks, and to countries like Tanzania to set up national electronic logistics management systems.
Speed up product flow through the supply chain
- Map current supply chain processes to understand where duplication or wastage is happening. Process mapping provides insight into the systems and processes involved in product movement through the supply chain, who is doing what and when, and the time spent. It is a first step to understand duplication in efforts, wastage in time and resources, as well as key bottlenecks, and is seen as useful in health care quality improvement projects.42 Subsequently, once the bottlenecks in the current processes are identified, the next step is to redesign the supply chain processes to address these inefficiencies.
- Utilize network optimization tools to understand the optimal infrastructure for a given supply chain in a specific context. Whilst infrastructure changes can be expensive, in the longer term they should drive down costs and improve the experience for all those involved in the process, including most importantly the user. Network optimization is often coupled with redesigning the inventory and distribution rules of the system to further maximize benefits. Such design can carefully balance the needs of service, efficiency, and resilience in the supply chain.
Build and support a competent, professional supply chain workforce
- Use a systematic, sustainable approach to strengthen supply chain human resources in-country. The traditional approach to overcome limited supply chain capacity has been to provide technical training to staff working on supply chain functions, but this approach has limited, short-term impact with poor sustainability.28 Countries should instead strive to develop national systems and programs that can sustainably prepare and engage (through employment or outsourcing) the required supply chain workforce. This means understanding what competencies are required to manage and operate their supply chain, planning how these will be developed in the educational system, and ensuring the supply chain workers are explicitly considered throughout all aspects of the human resources cycle.43 The People that Deliver Initiative has recently developed a theory of change to support countries in this approach.28
- Foster and build strong leadership for supply chain management. Strong supply chain performance requires health sector leaders who understand the importance of the supply chain to achieving health outcomes, and supply chain leaders who can envision and drive transformational change. One example of a program that supports leadership to learn the necessary skills for supply chain managers is STEP (Strategic Training Executive Programme), which supports participants to develop their problem-solving skills and foster effective team-building approaches. STEP trained 76 participants from 15 countries between 2016 and 2017, and has since expanded.44
Capitalize on private sector supply chain capacity, where appropriate
- Supply chain operations are labor- and asset-intensive, require specialized technical expertise, and provide economies of scale through consolidation. In most countries, supply chain management is not a core business or comparative strength of governments or ministries of health. A policy that supports private sector engagement in the supply chain and leverages private sector capacities can increase performance while decreasing cost per unit delivered.37,12 Third-party logistics providers can be contracted to provide specific supply chain services, such as procurement, customs clearance, warehousing, or distribution. In addition, “fourth party logistics providers” can be used to manage an array of third-party providers and services to provide comprehensive supply chain solutions.
- Contract management and oversight are both critical prerequisites for private-sector run transport and distribution. Many countries lack sufficient mechanisms and capacities in these areas. It is important to start by assessing capacity in the government for contract management and for defining and enforcing contract provisions and performance expectations, as well as other mechanisms for effective private sector engagement. Seeking support and building capacity where gaps exist will be a key first step.
- Conduct an in-depth, cost-risk-benefit and private-sector capability analysis. This should include a thorough costing analysis of the existing government-owned transport and distribution system, taking into account hidden costs such as asset depreciation and staff time, and understanding the private sector operators’ geographical reach and costs. Where it makes sense to engage the private sector (either in selected regions or nationally), getting top-level ownership of the process within the government, including the finance ministry, is critical to ensure analysis is utilized and the solutions move forward.
It is recommended that programs implementing supply chain management include the following indicators:
- Percentage of facilities stocked out, by family planning product or method offered, on the day of the assessment (reporting day or day of visit)45
Additional Reading
Additional Reading
General Supply Chain Management Guidance: MDS-3: Managing Access to Medicines and Health Technologies. 2012. Management Sciences for Health. https://www.msh.org/resources/mds-3-managing-access-to-medicines-and-health-technologies
Reproductive Health Commodity Security and Data Visibility: Reproductive Health Supply Coalition tools page: https://www.rhsupplies.org/activities-resources/tools/
Human Resources for Health Supply Chains: People that Deliver resource page: https://peoplethatdeliver.org/ptd/resources
Outsourcing and Engaging Private Sector: Private Sector Engagement: A Guidance Document for Supply Chains in the Modern Context. 2014. United Nations Commission on Life-Saving Commodities, Technical Reference Team on Private Sector Engagement. http://www.lifesavingcommodities.org/wp-content/uploads/2014/08/UNCoLSC-Private-Sector-Engagement-Guidance-Document_revised-Oct-2014-1.pdf
References
- Mukasa B, Ali M, Ferron M, Van de Weerdt R. Contraception supply chain challenges: a review of evidence from low- and middle-income countries. Eur J Contracept Reprod Health Care. 2017;22(5):384-90. http://doi.org/10.1080/13625187.2017.1394453
- EngenderHealth. The SEED assessment guide for family planning programming. New York: EngenderHealth; 2011. https://www.engenderhealth.org/files/pubs/family-planning/seed-model/seedassessment-guide-for-family-planning-programming-english.pdf. Accessed April 3, 2020.
- Track20. Monitoring annual progress. Glastonbury, CT: Avenir Health; 2020. http://www.track20.org/pages/data_analysis/core_indicators/progress_report.php. Accessed April 3, 2020.
- Reproductive Health Supplies Coalition (RHSC). Global family planning visibility and analytics network. Resources: supply chain image. Brussels, Belgium: RHSC; 2020. https://www.rhsupplies.org/fileadmin/uploads/rhsc/Tools/Global-FP-VAN/SCM_HIP_Figure_2.png. Accessed April 16, 2020.
- High Impact Practices in Family Planning (HIPs). Family planning high impact practices list. Washington, DC: USAID; 2019. https://fphighimpactpractices.org/high-impact-practices-in-family-planning-list/. Accessed April 3, 2020.
- Mercer Management Consulting. Contraceptive Availability Study: Methodology and Key Findings. Mercer Management Consulting; 2005.
- Ali M. Family planning evidence brief: ensuring contraceptive security through effective supply chains. Geneva: World Health Organization; 2017. http://ec2-54-210-230-186.compute-1.amazonaws.com/wpcontent/uploads/2017/07/FP-Evidence-supply-chains-FINAL-07.10.17.pdf. Accessed April 6, 2020.
- Wang, W, Wang S, Pullum T, Ametepi P. How Family Planning Supply and the Service Environment Affect Contraceptive Use: Findings from Four East African Countries. Calverton, MD: ICF International; 2012. https://dhsprogram.com/pubs/pdf/AS26/AS26.pdf. Accessed April 6, 2020.
- Wang W, Winter R, Mallick L, Florey L, Burgert-Brucker C, Carter E. The Relationship Between the Health Service Environment and Service Utilization: Linking Population Data to Health Facilities Data in Haiti and Malawi. Rockville, MD: ICF International; 2015. https://www.dhsprogram.com/pubs/pdf/AS51/AS51.pdf. Accessed April 6, 2020.
- Skiles MP, Cunningham M, Inglis A, et al. The effect of access to contraceptive services on injectable use and demand for family planning in Malawi. Int Perspect Sex Reprod Health. 2015;41(1):20-30. http://doi.org/10.1363/4102015
- Shiferaw S, Spigt M, Seme A, et al. Does proximity of women to facilities with better
choice of contraceptives affect their contraceptive utilization in rural Ethiopia? PLoS ONE. 2017;12(11):e0187311. https://doi.org/10.1371/journal.pone.0187311 - [impact]Hasselback L, Dicko M, Viadro C, Ndour S, Ndao O, Wesson J. Understanding and addressing contraceptive stockouts to increase family planning access and uptake in Senegal. BMC Health Serv Res. 2017 May 26;17(1):373. http://doi.org/10.1186/s12913-017-2316-y
- [impact]Reproductive Health Supplies Coalition (RHSC). RFP Addendum #2017-045. Global Family Planning Visibility Analytics Network. Brussels, Belgium: RHSC; 2017. https://www.rhsupplies.org/fileadmin/uploads/rhsc/Tools/Global-FP-VAN/
RFP_Addendum.pdf. Accessed April 3, 2020. - [impact]Cai J, Liu X, Xiao Z, Liu J. Improving supply chain performance management: a systematic approach to analyzing iterative KPI accomplishment. Decision Support Systems. 2009;46(2):512-521. http://doi.org/10.1016/j.dss.2008.09.004.
- [impact]Stephens, S. Supply chain operations reference model version 5.0: a new tool to improve supply chain efficiency and achieve best practice. Information Systems Frontiers. 2001;3(4):471-476. https://doi.org/10.1023/A:1012881006783
- [impact]Nigeria, Kaduna State Government; Bill & Melinda Gates Foundation; Pamela Steele Associates (PSA) Limited. 1ST quarter report of the Kaduna State Public Health Supply Chain Transformation Project. Kaduna, Nigeria: 2017. https://kdsg.gov.ng/wp-content/uploads/2018/05/1st_Quarter-KadunaStatePupplicHealthSupplyChainTransformationProject_Approved.pdf. Accessed April 3, 2020.
- [impact]Titze C, McNeill W, De Muynck, B. Gartner. Magic quadrant for multienterprise supply chain business networks. Gartner.com. November 15, 2018. Accessed April 6, 2020. https://www.gartner.com/doc/reprints?id=1-5SEIK3R&ct=181115&st=sb
- [impact]Alayande A, Mamman-Daura F, Adedeji O, Muhammad AZ. Midwives as drivers of reproductive health commodity security in Kaduna State, Nigeria. Eur J Contracept Reprod Health Care. 2016;21(3):207-212. http://doi.org/10.3109/13625187.2015.1137280
- [impact]Mwencha M, Rosen JE, Spisak C, Watson N, Kisoka N, Mberesero H. Upgrading supply chain management systems to improve availability of medicines in Tanzania: evaluation of performance and cost effects. Glob Health Sci Pract. 2017;5(3):399-411. https://doi.org/10.9745/GHSP-D-16-00395
- [impact]Wehlage, CJ, Fletcher C.. Multi-tier distribution channels: moving from three tier to two tier. Stamford, CT: Gartner Research; 2008.
- [impact]Lee BY, Connor DL, Wateska AR, et al. Landscaping the structures of GAVI country vaccine supply chains and testing the effects of radical redesign. Vaccine. 2015;33(36):4451–4458. http://doi.org/10.1016/j.vaccine.2015.07.033
- [impact]Shittu E, Harnly M, Whitaker S, Miller R. Reorganizing Nigeria’s vaccine supply chain reduces need for additional storage facilities, but more storage is required. Health Aff (Millwood). 2016;35(2):293–300. http://doi.org/10.1377/hlthaff.2015.1328
- [impact]Vledder M, Friedman J, Sjöblom M, Brown T, Yadav P. Improving supply chain for essential drugs in low-income countries: results from a large scale randomized experiment in Zambia. Health Syst Reform. 2019;5(2):158-177. http://doi.org/10.1080/23288604.2019.1596050
- [impact]Yadav P. Health product supply chains in developing countries: diagnosis of the root causes of underperformance and an agenda for reform. Health Syst Reform. 2015;1(2):142-154. http://doi.org/10.4161/23288604.2014.968005
- [impact]Peffer D. Nice example of a successful multi-partners collaboration. Posted July 2019. Accessed April 3, 2020. https://www.linkedin.com/posts/dimitri-peffer_in-mozambique-were-supporting-warehousing-activity-6557493446318395392-aN_7/
- [impact]Lee BY, Haidari LA, Prosser W, et al. Re-designing the Mozambique vaccine supply chain to improve access to vaccines. Vaccine.2016;34(41):4998-5004. http://doi.org/10.1016/j.vaccine.2016.08.036
- [impact]Lebetkin E, Orr T, Dzasi K, et al. Injectable contraceptive sales at licensed chemical seller shops in Ghana: access and reported use in rural and periurban communities. Int Perspect Sex Reprod Health. 2014;40:21–27. http://doi.org/10.1363/4002114
- [impact]People that Deliver. Building human resources for supply chain management: theory of change. Copenhagen, Denmark: People that Deliver; 2018. https://peoplethatdeliver.org/ptd/resources/building-human-resources-supply-chain-management-theory-change. Accessed April 3, 2020.
- [impact]Steele, P. GAVI Alliance Immunization Supply Chain Strategy: Assessment of the Human Resources Landscape for Immunization Supply Chain Management. Copenhagen, Denmark: UNICEF; 2016. https://peoplethatdeliver.org/ptd/sites/default/files/resource_contents_files/Assessment%20of%20the%20HR%20Landscape%20for%20Immunization%20Supply%20Chain%20Management.pdf. Accessed April 6, 2020.
- [impact]USAID | DELIVER PROJECT, Task Order 4. Health Logistics in Nepal: Two Decades of Investments in Public Health Supply Chain Management: How Access to Supplies Improved Health Outcomes in Nepal. Arlington, VA: John Snow, Inc., USAID | DELIVER PROJECT, Task Order 4; 2014. https://apps.who.int/medicinedocs/documents/s21574en/s21574en.pdf. Accessed April 6, 2020.
- [impact]Taddesse D, Hoza S, Seifu T, Cochrane L. Building blocks for enhancing personnel performance: activities, best practices and lessons learned from Ethiopia. J Pharm Policy Pract. 2014;7 Suppl 1:S1-2. https://doi.org/10.1186/2052-3211-7-S1-O2
- [impact]People that Deliver. Namibia’s integrated actions to improve the health supply chain management workforce. Copenhagen, Denmark: People that Deliver; 2015. https://peoplethatdeliver.org/ptd/sites/default/files/country-partnership-files/Namibia%20Synthesis%20Report_FINAL_0.pdf. Accessed April 6, 2020.
- [impact]Cometto G, Babar Z-U-D, Brown A, Hedman L, Campbell J. “Health supply chain personnel: an integral part of the health workforce.” J Pharm Policy Pract. 2014;7(S1). http://doi.org/10.1186/2052-3211-7-s1-i1
- [impact]High-Impact Practices in Family Planning (HIPs). Leaders and managers: making family planning programs work. Washington, DC: USAID; 2015. https://fphighimpactpractices.org/briefs/leaders-and-managers. Accessed April 6, 2020.
- [impact]Dalberg Global Development Advisors; MIT-Zaragoza International Logistics Program. Private sector role in health supply chains: review of the role and potential for private sector engagement in developing country health supply chains. New York: Rockefeller Foundation; 2008. https://apps.who.int/medicinedocs/documents/s16323e/s16323e.pdf. Accessed April 6, 2020.
- [impact]Lydon P, Raubenheimer T, Arnot-Krüger M, Zaffran M. Outsourcing vaccine logistics to the private sector: The evidence and lessons learned from the Western Cape Province in South-Africa. Vaccine. 2015;33(29):3429–3434. http://doi.org/10.1016/j.vaccine.2015.03.042
- [impact]Agrawal P, Barton I, Dal Bianco R, Hovig D, Sarley D, Yadav P. Moving medicine, moving minds: helping developing countries overcome barriers to outsourcing health commodity distribution to boost supply chain performance and strengthen health systems. Glob Health Sci Pract. 2016;4(3):359-365. http://dx.doi.org/10.9745/GHSP-D-16-00130
- [impact]High-Impact Practices in Family Planning (HIPs). Drug shops and pharmacies: sources for family planning commodities and information. Washington, DC: USAID; 2013. https://fphighimpactpractices.org/briefs/drug-shops-and-pharmacies. Accessed April 6, 2020.
- [impact]High-Impact Practices in Family Planning (HIPs). Family planning vouchers: a tool to boost contraceptive method access and choice. Washington, DC: USAID; 2019. https://fphighimpactpractices.org/briefs/family-planning-vouchers. Accessed April 6, 2020.
- Hurkchand H. Technical review of public health supply chain assessment tools: an analysis of major tools and approaches, 2019. Oral presentation at: Global Health Supply Chain Summit; November, 2019; Johannesburg, South Africa. ghscs.com/wp-content/
uploads/2019/11/160-ISG_Assessments_Nov2019.pptx. Accessed April 6, 2020. - Reproductive Health Supplies Coalition (RHSC). Global family planning visibility analytics network. Brussels, Belgium: RHSC; 2020.
https://www.rhsupplies.org/activities-resources/tools/global-fp-van/. Accessed April 3, 2020. - Antonacci G, Reed J, Lennox L, Barlow J. The use of process mapping in healthcare quality improvement projects. Health Serv Manage Res. 2018;31(2):74-84. http://doi.org/10.1177/0951484818770411
- Seifman R, Bailey R, Hasselberg E. Applying the HRH Action Framework to develop sustainable excellence in the health supply chain workforce. Chapel Hill, NC: Intrahealth International, CapacityPlus Project; 2013. https://www.capacityplus.org/technical-brief-12/index.html. Accessed April 6, 2020.
- Gavi. IFPW and Gavi expand leadership training for a stronger supply chain. Geneva: Gavi; 2018. https://www.gavi.org/news/media-room/ifpw-and-gavi-expand-leadership-training-stronger-supply-chain. Accessed April 3, 2020.
- Reproductive Health Supplies Coalition (RHSC). Harmonized suite of indicators to measure stockouts and availability of contraceptives, version 1.0. Indicator B1. Arlington, VA: JSI Research and Training Institute, Inc.; 2015. https://www.rhsupplies.org/uploads/tx_rhscpublications/Harmonized_Suite_of_Indicators.pdf. Accessed April 3, 2020.
Suggested Citation
High Impact Practices in Family Planning (HIPs). Supply chain management: Investing in the supply chain is critical to achieving family planning goals. Washington, DC: HIPs Partnership; 2020 Apr. Available from: http://fphighimpactpractices.org/briefs/supply-chain-management/
Acknowledgements
This brief was updated by Julia White, Kate Wright, Kevin Pilz and Prashant Yadav with input from Martyn Smith, Jennie Greaney, Samantha Lemieux and Laura Raney. It was updated from a previous version authored by Lilia Gerberg, Ellie Bahirai, Leslie Patykewich, and Linda Cahaelen. Critical review and helpful comments were provided by Moazzam Ali, Michal Avni, Martha Brady, Andrew Brown, Tamar Chitashvili, Peter Fajans, Bamikale Feyisetan, Spiros Paulo Fournogerakis, Roy Jacobstein, Rita Kabra, James Kiarie, Asa Cuzin Kihl, Erin Mielke, Emmanuel Nfor, Japheth Ominde, Leslie Patykewich, Chloe Peebles, Anne Pfitzer, Sara Stratton, Anand Sinha, and Caitlin Thistle.
The following organizations contributed to the development of this brief: Abt Associates, Chemonics, DKT/Brazil, David and Lucile Packard Foundation, EngenderHealth, ExpandNet, FHI 360, Futures Group, FP2020, Georgetown University/Institute for Reproductive Health, Harvard Medical School, International Planned Parenthood Federation, IntraHealth International, Jhpiego, John Snow, Inc., Johns Hopkins Bloomberg School of Public Health Center for Communication Programs, Management Sciences for Health, Marie Stopes International, PATH, Pathfinder International, Palladium, Population Council, Population Services International, Reproductive Health Supplies Coalition, University Research Co., LLC, United Nations Population Fund, U.S. Agency for International Development, and World Health Organization.
The World Health Organization/Department of Reproductive Health and Research has contributed to the development of the technical content of these documents which are viewed as a summary of evidence and field experience. It is intended that these briefs are used in conjunction with WHO Family Planning Tools and Guidelines: http://www.who.int/topics/family_planning/en/.
Provide Comments
To provide comments on this brief, please fill out the form on the Community Feedback page.